Kelly Spill did not cry when she was diagnosed with stage III rectal cancer at the age of 28, CNN reported.
She kept her emotions in check when her surgeon told her she might not be able to have more children — radiation treatment can significantly affect fertility — and that she might have to wear a colostomy bag to collect waste after surgery.
"I didn't cry either time," said Spill, who was newly engaged at the time and only a few months after giving birth.
"But then I asked [the doctor], 'Will I still be able to go to Switzerland this summer to get married?' And he said, 'Oh, absolutely not.' And that really broke me," she said. "That's when I really realized that my life had completely changed."
After the birth of her son Jace, she and her fiancé had planned to elope to Switzerland to get married. But after her cancer diagnosis, they decided on a quick winter wedding in their hometown.
Now, five years later, not only has Spill given birth to another baby — Jace now has a little sister named Mia — but she and her husband are expecting their third child.
Spill, who has no family history of colorectal cancer, was among more than 100 adults in the US who completed cancer treatment in a new study using only the immunotherapy drug dostarlimab, and she said the experience changed her life.
When Spill was diagnosed in 2020, her treatment plan included heavy chemotherapy drugs, radiation therapy, and invasive surgery. But just before she scheduled her first chemotherapy appointment, she was offered the opportunity to participate in the new study. When she realized that the approach, which uses only dostarlimab, would be gentler on her body, she signed up immediately.
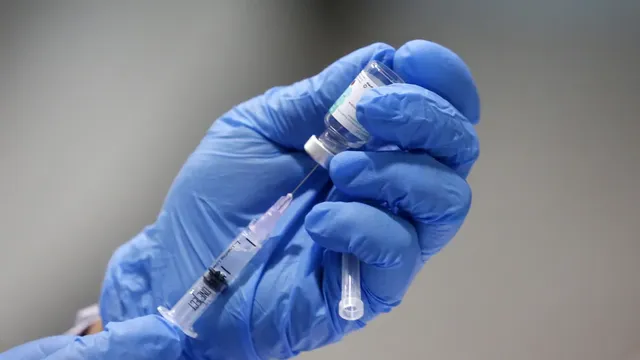
Immunotherapy is a form of cancer treatment that uses a person's own immune system to attack and fight the disease. Dostarlimab, developed by the pharmaceutical company GSK and sold under the brand name Jumperli, has been shown in previous studies to virtually eliminate solid tumors in people with rectal cancer. Last year, the US Food and Drug Administration designated dostarlimab as a "breakthrough therapy" for the treatment of certain types of rectal cancer.
But the new study, published last week in the New England Journal of Medicine, found that immunotherapy works not only in advanced rectal cancer, but also in other types of cancer, allowing patients to avoid surgery and other more invasive treatments.
Spill received 30-minute intravenous infusions of dostarlumab at a medical facility every three weeks and reported no adverse side effects.
"It took four treatments before I realized that the tumor had shrunk by half, and after the ninth treatment, the tumor disappeared completely. That's when they told me I was cured of cancer," Spill said.
"Then they told me I didn't need to undergo radiation or surgery, and that was one of the happiest days of my life because I knew I could continue planning to have a baby," she added. "This clinical trial completely changed my life... and it's like a miracle."
"It's suitable for every type of cancer in the body."
The new study included 117 cancer patients divided into two groups. One group included people with advanced rectal cancer, and the other included people with other types of solid tumors, such as colon, stomach, bladder, and prostate cancer.
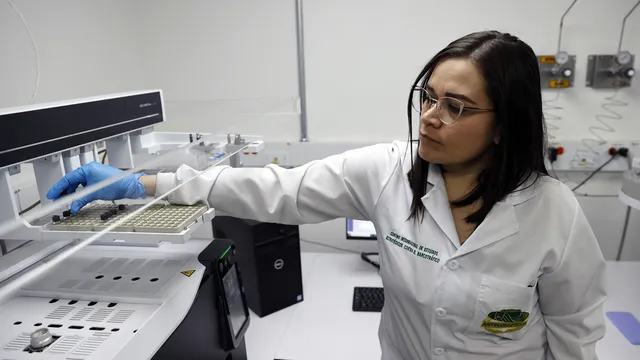
All participants had cancer mismatch repair deficiency, or dMMR, which means that their tumor cells are cells with a deficiency in mismatch repair. These types of cells usually have many DNA mutations and, according to the study, are thought to affect up to 3% of all solid tumors in the early stages.
"We are constantly faced with the breakdown of our cells, and with the help of DNA, we can repair this ongoing damage to cells over time," said Dr. William Dahut, chief scientific officer of the American Cancer Society, who was not involved in the new study. "But if there is a deficiency in this repair process, then you get a greater number of abnormalities in the DNA, which we call mutations. And we know that people with a greater number of mutations often have a greater ability to respond to immunotherapy."
This ability to respond to immunotherapy was demonstrated in the new study.
Data were collected between December 2019 and April 2025, with 103 participants completing treatment in both groups. They received intravenous infusions of dostarlumab for six months and were monitored for two years as part of a follow-up to a previous study.
"The first study we published in 2022 showed that we could do this in patients with rectal cancer whose tumors had a mutation associated with mismatch repair deficiency, and what was remarkable was that in 100% of patients, the tumors disappeared — something has never been achieved before in oncology," said Dr. Luis Diaz, head of the solid tumor oncology department and gastroenterological oncologist at Memorial Sloan Kettering Cancer Center and author of the new study.
Now, "what we just published shows two things. These rectal cancer patients remain 100% in remission, with nearly 50 patients responding completely, but the effect is lasting. Durability is important because the tumor has disappeared for up to five years or more in some patients, allowing them to return to their normal lives," Diaz explained.
"The second part of the story is that this is not just true for rectal cancer," he added. "This is true for any type of cancer in the body, as long as the tumor has a genetic mutation."
The researchers found that 80% of study participants who completed treatment with only immunotherapy with dostarlumab did not require surgery, radiation, or chemotherapy after six months of treatment. The results were presented at the American Association for Cancer Research's annual meeting in 2025.
"In all patients who had a clinical complete response, the organs were preserved without additional therapy. Three patients with rectal cancer subsequently conceived and gave birth to healthy children, which would not have been possible with standard treatment for rectal cancer," the researchers wrote in the study.
Two years later, about 92% of all patients in both groups had no recurrence of cancer. The disease recurred in only five patients in both groups: in one person with rectal cancer, the tumor reappeared, and in the other four, the recurrence was only in the lymph nodes.
Although 65% of people who received at least one dose of dostarlimab reported side effects, most were mild and included fatigue, rash, or irritation at the infusion site, or itching. No participants in either group died during the study.
"For patients, this is incredible because we can effectively eliminate their disease with minimal toxicity," said Dr. Andrea Cercek, a gastroenterology oncologist at Memorial Sloan Kettering Cancer Center and author of the new study.
"Our goal in oncology is always to cure, but often many of our treatments leave patients with certain impairments," she added. "What we're seeing with this treatment is that we can skip standard therapies—radiation, chemotherapy, and, most importantly, surgery — in 80% of patients with minimal toxicity, allowing them to feel well, with intact organs, and to lead as normal a life as possible."
The researchers write that although these results are encouraging, "larger studies are needed to confirm the long-term benefit of this treatment, especially in patients with non-rectal tumors." But the new study "lays the groundwork" for the next steps.
A new era in cancer treatment
Chemotherapy, radiation therapy, and surgery are usually the main components of treatment plans for most types of cancer, and these approaches have been widely used for decades. For example, the first radical mastectomy for breast cancer was performed in 1882. The first use of radiation therapy to treat cancer was described in 1899. In the 1950s, scientists announced the first complete cure of a solid tumor in a human using chemotherapy.
But in recent years, there has been "more and more evidence" that immunotherapy may be effective in people with tumors that lack mismatch repair, according to Dr. Stacy Cohen, a physician at the Fred Hutchinson Cancer Center in Seattle, who was not involved in the new study.
"This is extremely innovative because historically we have considered surgery to be the primary treatment for localized cancer, with all other additional therapies aimed at reducing the risk of recurrence. So, as we enter an era where non-surgical treatment may become the new standard of care with long-lasting and effective therapies, this is very exciting for both patients and doctors," Cohen said.
"But we know that not all patients will have such an incredible response, even if they have the right biomarker," she added. "And that's simply because there can be nuances in people's tumors, and one treatment is not right for everyone."
Cohen added that she had "two caveats" regarding the results of the new study.
"The first is that immunotherapy did not work for all patients in this study," she noted. Second, "this is only true for a strictly selected group of patients with dMMR/MSI tumors. It is very important that this biomarker be tested before considering immunotherapy, as this type of treatment will not work in most patients."
For cancer patients, it is important that their tumors are genetically consistent because this process can help guide treatment decisions by identifying which specific mutations may be causing the cancer, Dahut said.
Once these mutations are identified, patients can understand whether any new and emerging immunotherapies may help them by targeting those mutations.
"This is one of the reasons why patients should have their tumors sequenced at diagnosis, because it's not something you would necessarily know you have, but if you do, then your treatment — even at initial diagnosis or in recurrent or advanced disease — would have significantly more options," Dahut said.
With immunotherapies, "it's impressive not only that we're seeing complete responses, but that the responses appear to be durable," he added.
Increase in cancer among young adults
The new study comes at a time when cases of colorectal cancer are increasing among younger adults. A report published in 2023 by the American Cancer Society shows that the proportion of colorectal cancer cases among adults under 55 has risen from 11% in 1995 to 20% in 2019.
When Cercek and her colleagues began the new study, she said their goal was to find less invasive treatment options for these younger people with colorectal cancer.
"One of the reasons for the design of this study was that we were seeing so many young patients in the clinic and how harmful our treatment could be. That motivated me in my research for a long time. Even before this study of immunotherapy in mismatch repair-deficient tumors, we were trying to improve treatment for early-stage disease for all of our patients, but especially for young adults," Cercek said.
Spill expressed hope that other young adults with rectal cancer will ask their doctors about clinical trials that may be beneficial to them—especially with the development and advancement of cancer treatments, which are becoming less invasive.
"A lot of us think of clinical trials as a last resort, and I think we need to get rid of that stigma because it really shouldn't be that way. You never know what might help you," Spill said.
"There is an increase in colorectal cancer in men and women at a young age. And fertility doesn't just affect women, it affects men too," she added. "When you're young and you're diagnosed with a cancer that you thought only happened in old age, it's scary."
Signs and symptoms of colorectal cancer may include changes in bowel habits, rectal bleeding or blood in the stool, cramps or abdominal pain, weakness and fatigue, and weight loss.
But Spill warned that these symptoms can often be overlooked or confused with other health problems in young adults. Her symptoms included constipation, bloody stools, and abdominal pain, but because they appeared after the birth of her first child, doctors told her they were related to childbirth and internal hemorrhoids.
"One day I went to the bathroom and looked down and you would have thought I had started my period, but it definitely wasn't. That's when I started to get really worried," Spill said.
When she noticed large amounts of blood again, she took pictures and showed them to her primary care physician. The doctor immediately scheduled a colonoscopy, which led to the cancer diagnosis.
"Standing up for yourself is so important," Spill said. "If I hadn't insisted, I don't know where I would be now, especially as a new mother."
When Spill now thinks about her 28-year-old self, the woman who burst into tears in the doctor's office after being told to cancel her plans to escape to Switzerland, she has one message: "Take a deep breath and trust the process." |BGNES

 Breaking news
Breaking news
 Europe
Europe
 Bulgaria
Bulgaria