Far from being a simple isolated mutation, cancer is now seen as the result of cellular competition.
Some protective cells manage to slow down or even eliminate their precancerous neighbors—a promising avenue for prevention.
For a long time, the dominant view of cancer consisted of a simple equation: a cell undergoes genetic mutation, evades the body's control mechanisms, and begins to multiply uncontrollably.
Gradually, it forms a tumor, whose cells break away and reach other organs. But in recent years, this "canonical" approach to the disease has been seriously shaken, according to an article in The Economist magazine.
In fact, the so-called "driver" mutations that promote the development of cancer are not rare in our bodies, but they do not systematically cause serious diseases.
They are found, for example, in about a quarter of the cells of skin that appears normal.
After the age of 40, more than half of the esophagus and nearly 10% of the stomach lining are already covered with cells carrying these genetic abnormalities.
These areas, which are obviously at risk, are also found in the colon, lungs, and ovaries.
Why, then, do these cells, which appear ready to become malignant, not systematically form tumors?
The answer that emerges is surprising. Mutated cells do not actually live alone; their fate also depends on their neighboring cells, which sometimes possess beneficial mutations that limit the spread of the more dangerous ones.
In this biological microcosm, competition is fierce, and it appears that strengthening healthy "protective" cells may become a promising strategy for cancer prevention.
This idea stems from a new understanding of tissue dynamics. Since every cell division is accompanied by random mutations, the surface layers of our organs (skin, esophagus, stomach) become a genetic battlefield.
The most adaptable cells survive and push the less adaptable ones out of the tissue, like in a constant game of musical chairs.
Precancerous cells themselves can be displaced by other, better-armed cells.
Experiments conducted on mice even show that miniature tumors that are still in the embryonic stage can be neutralized in this way.
This competition may explain why some genetic changes appear early in life but do not always lead to cancer.
Successive blood samples show that the number of potentially risky cells varies over time, with some disappearing and others recovering. Can medicine then direct this competition in favor of the most protective cells?
This is what British researchers at the Wellcome Sanger Institute attempted to do. Studying a common mutation of the PIK3CA gene, known to stimulate cell growth, they observed that the altered cells changed their metabolism to displace their neighboring cells.
Surprise: by giving mice metformin, a well-known anti-diabetic drug, they caused the same metabolic change in healthy cells, allowing them to compete on equal terms and prevent the mutated cells from taking over.
Conversely, a high-fat diet favors cancer cells, which is consistent with data linking obesity to esophageal cancer.
But this approach has its limitations, and "favorable" mutations are not universal: a change that is protective for the esophagus may be neutral or even dangerous for the skin. To map this complex genetic landscape, researchers are now relying on the CRISPR tool, which can quickly and precisely modify genes in living cells.
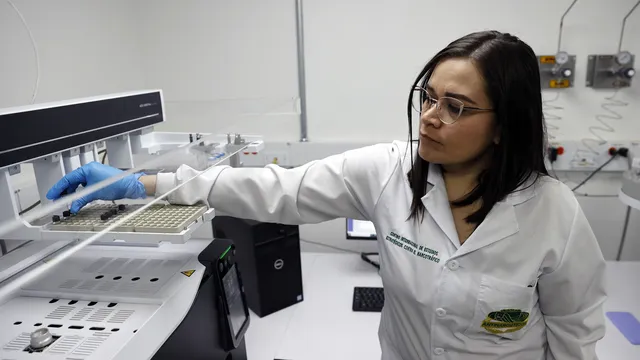
"We can study 15,000 genes in three months," says Phil Jones' team at the Wellcome Sanger Institute, delighted with a task that would previously have taken several years.
This research is also redefining our understanding of the root causes of cancer, as mutations are not the only factors that need to be monitored.
Environmental factors play a significant role, largely through chronic inflammation.
Many substances considered carcinogenic do not directly cause mutations, but maintain constant microinflammation that "awakens" precancerous cells.
Urbanization, pollution, recurrent gastric reflux, or chronic infections are all factors that promote inflammatory processes leading to tumor transformation.
A study published in Nature in 2023 highlights the role of air pollution in the development of lung cancer in non-smokers.
Prolonged exposure to fine particles causes inflammation of the lungs, which stimulates the growth of cells that already carry mutations.
Three years spent in a heavily polluted urban area are enough to trigger this process. A similar pattern is observed with solar radiation or certain chronic bacteria in the gut.
This discovery has led to an unexpected therapeutic approach: instead of targeting mutations alone, why not target the inflammation itself?
Blocking certain proteins in the immune system, such as interleukin-1, for example, has slowed the development of tumors in mice exposed to pollution.
These treatments could offer valuable protection to high-risk individuals, whether they are carriers of hereditary mutations, former smokers, or have already been treated for a first cancer.
This still emerging approach may herald an important shift that will transform the fight against cancer not only into a war to eradicate "bad" cells, but also into a strategy for balance that nourishes the vitality of protective cells and controls the body's inflammatory responses even before cancer develops.
This is a challenge that, with the increase in life expectancy and the growing incidence of cancer among the population, may become one of the most important medical challenges of the coming decades. | BGNES

 Breaking news
Breaking news
 Europe
Europe
 Bulgaria
Bulgaria